Welcome to the case study celiac disease answer key, your ultimate resource for understanding this complex condition. In this comprehensive guide, we will delve into the intricacies of celiac disease, from its definition and prevalence to its diagnosis and management.
Brace yourself for an in-depth exploration that will empower you with the knowledge to navigate the challenges of celiac disease.
Celiac disease is an autoimmune disorder triggered by gluten, a protein found in wheat, rye, and barley. It affects the small intestine, leading to a range of symptoms and potential complications. Understanding the disease is crucial for proper diagnosis and effective management.
Celiac Disease Overview
Celiac disease is an immune-mediated enteropathy triggered by the ingestion of gluten in genetically susceptible individuals. It is characterized by inflammation and damage to the small intestine, leading to malabsorption and a range of symptoms.The prevalence of celiac disease varies widely across geographic regions, with a higher prevalence in Europe and North America.
It is estimated to affect approximately 1% of the global population. The exact cause of celiac disease is unknown, but it is believed to involve a complex interaction between genetic, environmental, and immunological factors.
Genetic Basis of Celiac Disease
Celiac disease has a strong genetic component, with a heritability estimated to be around 80%. The major genetic risk factor for celiac disease is the presence of certain human leukocyte antigen (HLA) genes, specifically HLA-DQ2 and HLA-DQ8. These genes encode proteins that are involved in the presentation of gluten peptides to immune cells.
In individuals with celiac disease, these HLA proteins bind to gluten peptides and present them to immune cells, triggering an immune response that leads to inflammation and damage to the small intestine.
Clinical Manifestations of Celiac Disease: Case Study Celiac Disease Answer Key
Celiac disease is a chronic autoimmune disorder triggered by gluten ingestion in genetically susceptible individuals. It primarily affects the small intestine, leading to inflammation and damage to the intestinal villi. The clinical manifestations of celiac disease can vary widely, ranging from gastrointestinal symptoms to extraintestinal manifestations.
Gastrointestinal Symptoms
The most common gastrointestinal symptoms of celiac disease include:
- Abdominal pain and distension
- Chronic diarrhea
- Weight loss
- Nausea and vomiting
- Constipation
- Steatorrhea (fatty stools)
Extraintestinal Manifestations
In addition to gastrointestinal symptoms, celiac disease can also manifest in various extraintestinal organs and systems. These manifestations include:
- Dermatitis herpetiformis: A chronic skin condition characterized by itchy, blistering rashes
- Iron-deficiency anemia
- Osteoporosis and osteopenia
- Dental enamel defects
- Autoimmune thyroid disease
- Neurological symptoms (e.g., peripheral neuropathy, seizures)
- Infertility and miscarriage
Complications
Untreated celiac disease can lead to various complications, including:
- Malnutrition and nutrient deficiencies
- Increased risk of certain cancers (e.g., small intestine lymphoma)
- Infertility and pregnancy complications
- Osteoporosis and fractures
- Autoimmune disorders
Diagnosis of Celiac Disease
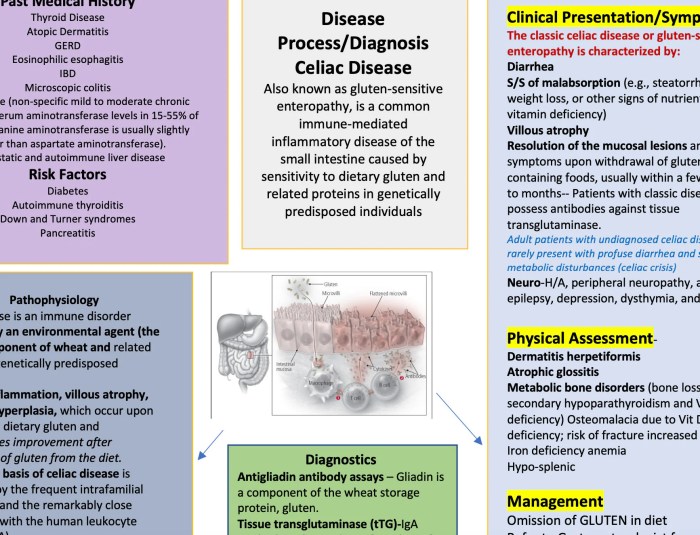
The diagnosis of celiac disease involves a combination of serologic testing, genetic testing, and endoscopic evaluation.
Serologic Testing
Serologic testing for celiac disease measures the levels of antibodies in the blood that are produced in response to gluten ingestion. These antibodies include:
- Anti-tissue transglutaminase (anti-tTG) antibodies
- Anti-endomysial antibodies (EMA)
- Anti-deamidated gliadin peptides (DGP) antibodies
A positive serologic test result suggests that the person has celiac disease, but it does not confirm the diagnosis.
Genetic Testing
Genetic testing for celiac disease can identify individuals who carry the HLA-DQ2 or HLA-DQ8 genes, which are associated with an increased risk of developing the disease. However, not all individuals who carry these genes will develop celiac disease, and some individuals who develop celiac disease do not carry these genes.
Endoscopic Evaluation
Endoscopic evaluation involves inserting a thin, flexible tube with a camera on the end (endoscope) into the small intestine to examine the lining of the intestine. During the procedure, the doctor may take biopsies of the intestinal tissue to look for signs of celiac disease, such as:
- Villous atrophy (flattening of the finger-like projections in the small intestine)
- Crypt hyperplasia (an increase in the number of cells in the crypts of the small intestine)
- Increased intraepithelial lymphocytes (IELs)
A positive endoscopic evaluation result confirms the diagnosis of celiac disease.
Management of Celiac Disease

Celiac disease, an autoimmune disorder triggered by gluten, requires lifelong management to prevent serious complications. The cornerstone of management is adhering to a strict gluten-free diet, supported by medications and lifestyle modifications.
Gluten-Free Diet
The gluten-free diet eliminates all foods containing gluten, a protein found in wheat, rye, and barley. This diet effectively prevents damage to the small intestine and allows it to heal. Strict adherence is crucial to manage symptoms, prevent complications, and improve overall health.
Challenges and Complications of Gluten-Free Diet, Case study celiac disease answer key
Adhering to a gluten-free diet can be challenging due to the widespread use of gluten in processed foods, cross-contamination, and social situations. Common complications include:
- Unintentional gluten ingestion due to hidden gluten sources or cross-contamination
- Nutritional deficiencies, such as iron, calcium, and vitamin D, due to the exclusion of gluten-containing foods
- Social isolation and anxiety related to dietary restrictions
Role of Medications
In some cases, medications may be prescribed to manage specific symptoms or complications of celiac disease. These include:
- Enzyme supplements:Gluten-digesting enzymes can help break down small amounts of gluten that may be accidentally ingested
- Immunosuppressants:These medications can suppress the immune response and reduce inflammation in the small intestine
- Corticosteroids:These medications can reduce inflammation and improve symptoms during acute flare-ups
Case Study Analysis
This section presents a comprehensive analysis of the case study on celiac disease, including a detailed overview of the clinical presentation, diagnostic approach, and management plan. A flowchart and differential diagnoses are also provided to enhance understanding of the diagnostic pathway and potential alternative diagnoses.
Case Study Details
| Case Study Detail | Description |
|---|---|
| Patient Demographics | Female, 35 years old, Caucasian |
| Chief Complaint | Chronic diarrhea, abdominal pain, and weight loss |
| Medical History | No significant medical history |
| Family History | Sister with celiac disease |
Clinical Presentation
- Gastrointestinal symptoms: Chronic diarrhea, abdominal pain, bloating, gas
- Constitutional symptoms: Weight loss, fatigue, weakness
- Dermatologic symptoms: Skin rash (dermatitis herpetiformis)
- Dental enamel defects
- Iron-deficiency anemia
- Osteopenia or osteoporosis
Diagnostic Approach
- Medical history and physical examination
- Blood tests: Serologic testing for anti-tissue transglutaminase (tTG) antibodies and anti-endomysial antibodies (EMA)
- Upper endoscopy with biopsy
- Genetic testing (HLA-DQ2/DQ8 haplotypes)
The diagnostic criteria for celiac disease require either a positive serologic test and a positive biopsy or a positive genetic test and a positive biopsy.

Management Plan
- Gluten-free diet
- Nutritional supplements (iron, calcium, vitamin D)
- Monitoring of symptoms and laboratory tests
- Regular follow-up with a healthcare provider
Differential Diagnoses
- Irritable bowel syndrome
- Inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
- Microscopic colitis (collagenous colitis, lymphocytic colitis)
- Small intestinal bacterial overgrowth (SIBO)
- Pancreatic insufficiency
- Lactose intolerance
Educational Resources and Support
Managing celiac disease effectively requires comprehensive patient education, access to reliable resources, and the support of a knowledgeable community.
Various organizations and online platforms provide valuable resources for celiac disease education and support:
Resources for Celiac Disease Education and Support
| Organization | Website | Resources |
|---|---|---|
| Celiac Disease Foundation | celiac.org | Information on celiac disease, diet, research, and support |
| National Celiac Association | nationalceliac.org | Educational materials, support groups, and advocacy |
| Beyond Celiac | beyondceliac.org | Research, education, and support for celiac disease and related disorders |
| Celiac Sprue Association | csaceliacs.org | Information, support, and advocacy for celiac disease patients |
| Gluten Intolerance Group | gluten.org | Research, education, and support for gluten intolerance and related disorders |
These organizations offer a range of resources, including:
- Educational materials (brochures, articles, videos)
- Support groups and online forums
- Dietitian and medical consultations
- Advocacy and legislative updates
- Research and clinical trial information
Patient education is crucial for effective celiac disease management. It empowers patients to:
- Understand their condition and its implications
- Follow a strict gluten-free diet
- Recognize and manage symptoms
- Make informed decisions about their healthcare
- Advocate for their rights and access to support
Support groups and online communities provide a valuable platform for celiac disease patients to connect with others who share their experiences. These communities offer:
- Emotional support and understanding
- Information and advice from peers
- Opportunities for social interaction
- A sense of belonging and community
- Advocacy and activism for celiac disease awareness and support
By accessing reliable educational resources and connecting with support networks, celiac disease patients can gain the knowledge, skills, and support they need to effectively manage their condition and live a healthy and fulfilling life.
FAQ Resource
What is the prevalence of celiac disease?
Celiac disease affects approximately 1% of the global population.
What are the common gastrointestinal symptoms of celiac disease?
Diarrhea, abdominal pain, bloating, and weight loss are common gastrointestinal symptoms of celiac disease.
What is the primary treatment for celiac disease?
The primary treatment for celiac disease is a strict gluten-free diet.
What are the potential complications of celiac disease?
Untreated celiac disease can lead to malnutrition, osteoporosis, and an increased risk of certain cancers.